Prefinals Longcase 1801006132
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
Chief complaints:
Reccurent episodes of vomitings associated abdominal pain since 2 months
History of present illness:
Patient was apparently asymptomatic 2 months back then he developed vomitings after 3-4 hours of taking food which was insidious in onset and is gradually progressive. The contents are food particles which is non blood stained and non bile stained. Aggrevated on taking food and no relieving factors. The vomiting are non projectile.Three to four episodes of vomitings each single day because of which patient avoided to eat food regularly and landed up in fatigue , weight loss .
Patient complaints of pain in the abdomen since 2 months which was diffused , squeezing type which is insidious in onset and gradually progressive non radiating to any other parts aggrevating and relieving factors
H/o giddiness ,nausea , fatigue , weakness , marked weight loss in the previous times ,
H/o constipation ,
Accidentally jaundice was diagnosed before 2 months for which he took medication
No H/o headache , fever , cold , cough , shortness of breath ,Orthopnea and PND
No H/o palpitations, chest pain , heart burn
No H/o hematemesis , heamatochesia , malena
Past history:
No similar complaints in past
No h/o Diabetes, hypertension , TB , Asthama and epilepsy
Family history:
No significant family history
Personal history:
Diet -mixed
Appetite- normal
Sleep - disturbed due to pain in abdomen
Bowel and bladder - bowel movements are irregular ( i.e once in every 5 -6 days) but bladder function is normal
Addictions- have habit of chewing tobbaco
Treatment history:
No significant treatment history
Vitals:
Temperature- afebrile
Pulse rate - 72bpm
RR - 15 cpm
Bp - 90/60 mm hg
Spo2 - 98
General Examination:
Patient is conscious, cohorent , cooperative well oriented to time place and person
He is thin built and under nourished
Pallor- present
Icterus- absent
Clubbing -absent
Cyanosis -absent
Lymphadenopathy -absent
Edema -absent
Physical Examination:
Sunken eyes due to loss of subcutaneous fat around orbits
Muscle wasting
Loss of weight and subcutaneous fat
Temporalis muscle atrophy
These all are suggestive of malnutrition
Systemic examination:
Abdominal examination
Inspection
The shape is scaphoid
Umbilicus is in central and inverted
No flank fullness
The skin is normal
Dilated loops with visible pulsations are seen
No dilated and engorged veins
No scars
Abdominal movements are normal
Palpation:
All the inspectory findings are confirmed
No local raise of temperature
A mass can be palpable in the right periumbilical region
No palpable liver an d spleen so , no hepatomegaly and splenomegaly
Percussion :
No fluid thrill
No shifting dullness
Ascultation:
Increased bowel sounds
CVS :
S1 S2 heard
No other murmurs
CNS :
No focal neurological deficit
Respiratory:
Normal vesibular breath sounds heard
Provisional diagnosis:
Abdominal obstruction
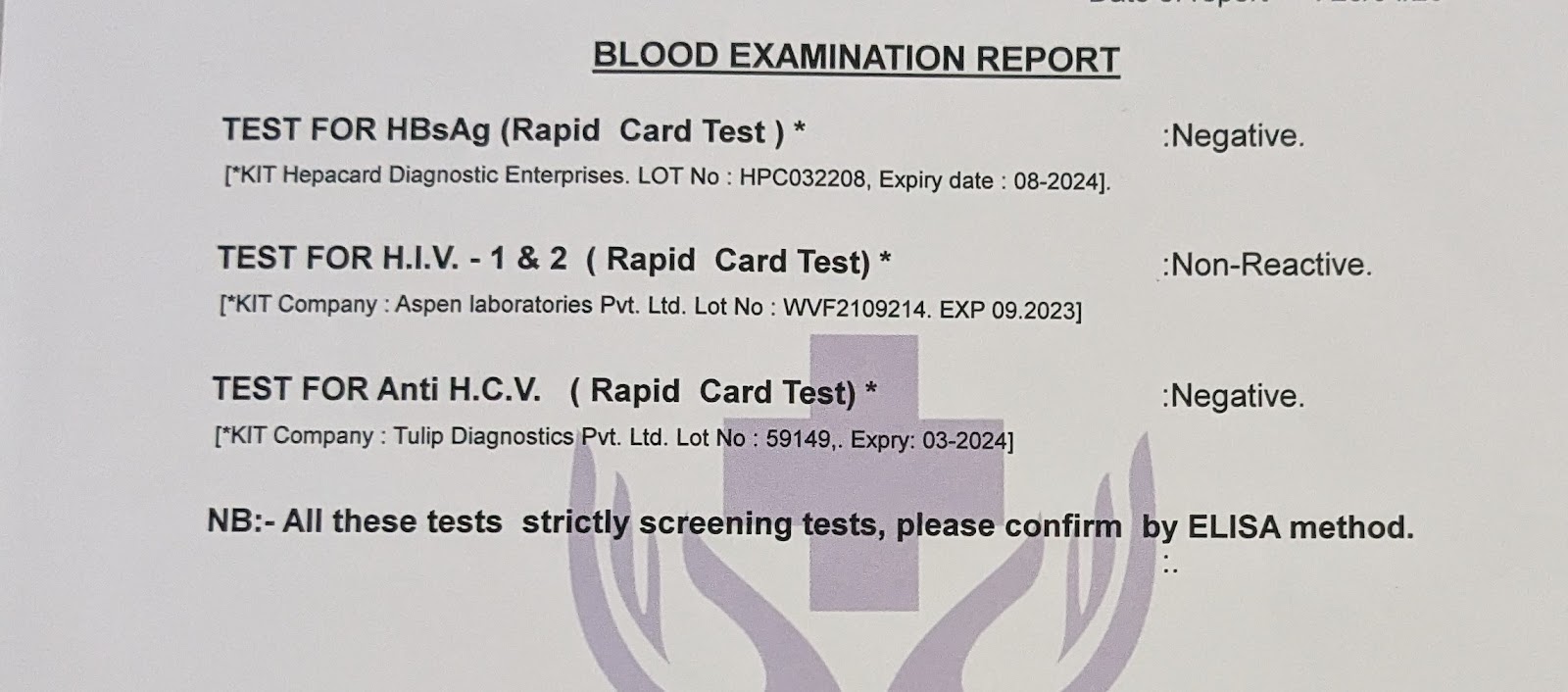
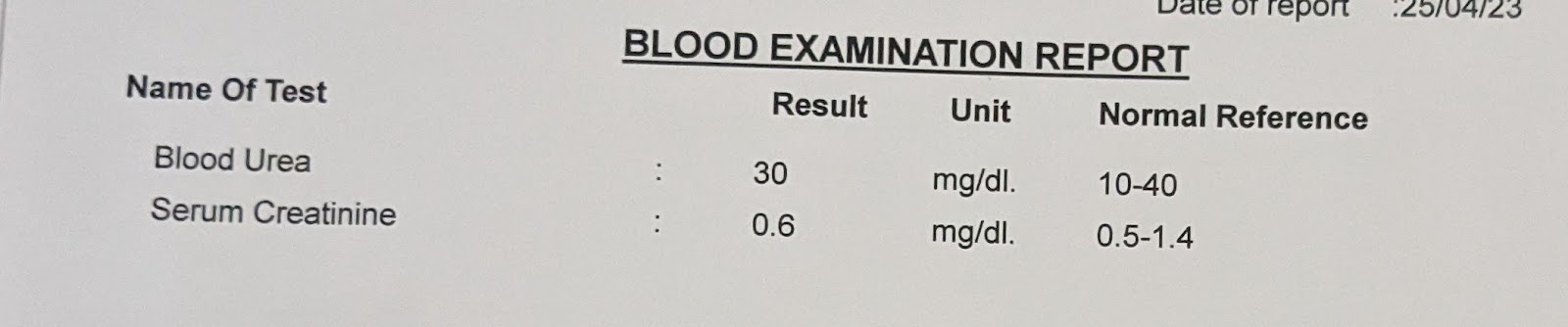
Investigations:
April 21
Diagnosis:
Intestinal Obstruction
Treatment:
Tab RAZO 40mg OD
Monitor vitals 6 hourly














Comments
Post a Comment